From a brochure to lower blood pressure
In a span of 3 years, we created an end to end service that help patients understand more about high blood pressure, create personalized goals to adjust lifestyle, and connect a Bluetooth enabled blood pressure monitor to the cloud. Proven effective by a one year pilot, we helped implement the program as standard of care in select locations at UI Health.
Client
UI Health
Date
September 2021
Services
Research + strategy + design
Duration
Multi-year, ongoing
Tags
Why is this a big deal?
According to the CDC, high blood pressure contributes to nearly 500,000 deaths per year in the United States. About half of all adults in the US have high blood pressure (108 million), yet only 1 in 4 have their condition under control. The condition disproportionately impacts lower income communities. Fortunately, and perhaps more frustratingly, high blood pressure is highly preventable with lifestyle adjustments and treatable with affordable medications, both solutions almost exclusively happen at home. Unfortunately though, the health care system as we know it struggles to extend beyond the walls of the hospitals and clinics. Changing lifestyle and ensuring patients adhere to treatment plans are notoriously challenging.
What's our approach?
Across the span of three years, we used our capabilities in a modular and iterative way. in 2021, The initial research led to an improved design of a booklet. We leveraged the tangibility of the booklet and the momentum garnered through the conversations with constituents to launch a pilot in 2022. In parallel, we started another round of research, strategy, and design to work out the service blueprint and assets needed for a feasible model. In 2023, we were lucky enough to implement the program while working on two other spin off projects we proposed based on prior research.

How did we tackle it?
Talk to patients
We started from the challenge of making a patient education brochure. But we quickly realized that while a brochure can be helpful, 'patient education' as a concept assumes that we are in the superior position talking at the patients, and that they don't 'know better'. What's more important, our true mission is to help patients better manage their own chronic conditions. That goes way beyond the narrow focus of education alone. This is one of our early, yet key, 'reframes'.
While patient education is a good starting point, we need mentors, coaches, advocates to engage (connect, motivate, and empower) with our patients and meet them where they are. This is important to support behavior change, especially for socially vulnerable patient communities.
Team Presentation August 2022
CONNECT
Patients need to first of all trust the person they are talking to and feel comfortable opening up. This requires a level of respect. This means to listen and allow them to ask questions, instead of talking at them. Patients from traditionally disadvantaged communities often feels more at ease spending time with someone who speaks their language and looks like them.
MOTIVATE
Not all patients are ready to make a change. It’s up to us to find the spark of motivation that drives the patient to challenge themselves and start on the journey of behavior change. Scare tactics about future heart failures don't always work. We need to apply motivational interviewing skills after we've gained trust.
EMPOWER
One size fit all recommendations about lifestyle doesn’t work when each patient has unique health and life situations. We need to uncover and consider these situations and co-create a personalized set of goals for each patient. The patient needs to own these goals and feel empowered to work on them.
Partner with physicians
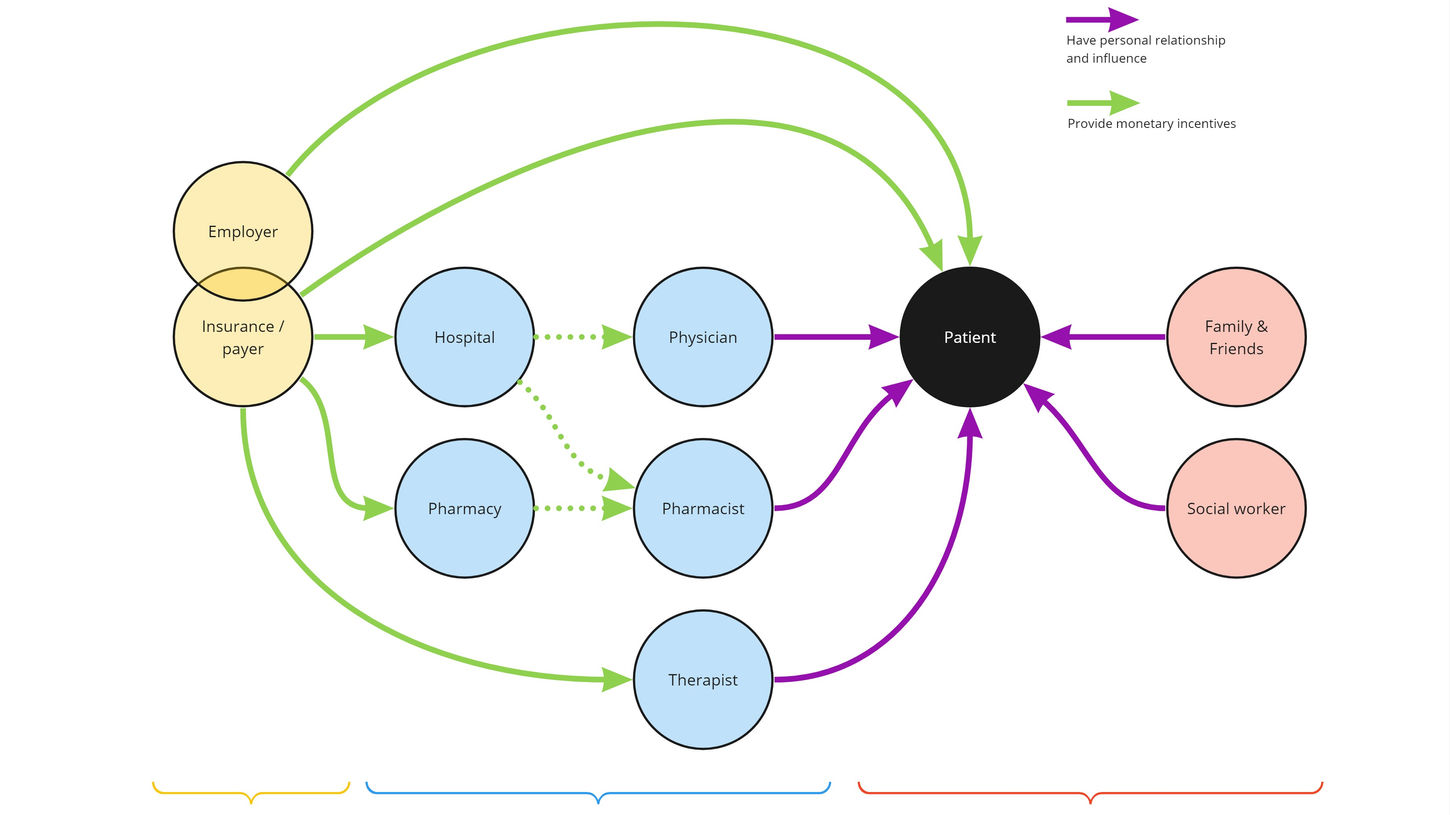
We knew early on that if we only went as far as treating physicians as stakeholders, we would fail. We need to become partners and co-develop the program from the get go. We had the pleasure to consult with many physicians. We also had the good fortune to start a long-term partnership with Dr. Bhrandon Harris. With guidance from physicians and supported by our own literary review, we found that an "interprofessional care team" was proven to work in helping patients manage their chronic conditions such as hypertension.
One of the biggest learnings we had from PCPs was that they would love to educate, connect, motivate, and empower each and every patient, but they simply can't afford to spend the time. And they not only don't mind other health care professionals to pitching in and help with engaging patients, they would LOVE the support.

Co-create with constituents
We mapped the constituents relevant to our program at UI Health, iterated around the patient journey, and started drawing dozens of different models and workflow diagrams about who should be involved in this care team, when and how the team could engage patients, what the work flow should look like if we want to support behavior change. We worked with 22 stakeholders over zoom and on Miro. The work was highly fluid and relentlessly collaborative. We often quickly clean up the diagram created from one session, and bring it directly to the next session to iterate.
Synthesize and prioritize with partners
We started with no limitations and envisioned teams of multi-disciplinary medical professionals dedicated to hypertension seeing patients in brand new clinics purposely built for them, supported and coordinated by a ubiquitous digital ecosystem internally and patient-facing. We also turned around and interrogated the ideas about feasibility. We knew any dramatic changes from the status quo will not only be financially non-viable, it will be met with resistance by the staff, more importantly, it wouldn't work for the patients when we demand them to go out of their way to engage.
The challenge to preserve the essence of the care team concept despite the constraints pushed us to think deeper. We keep coming back to the goal to connect, motivate and empower patients. The aha moment came to us when we realized that the minimum viable product (or MVP) of the interprofessional care team is not a team, it's one single person with the right expertise engaging the patient at the right time in the right space. As we continued to work closely with the cocreation partners, synergy started to emerge. Care Coordination with their passion to collaborate and the team of on-site social workers across multiple clinic locations became our partner to make the program a reality. We summarized the synergy in the following statement:
Anchor patient education
to existing embedded
patient engagement
models for Hypertension
-
Available to spend time with patients to educate about hypertension and health in general
-
Able to personalize HTN Action Plan for patients
-
Trusted to motivate and empower patients to make changes
-
Onsite for warm handoffs and just-in-time communication with providers as needed
-
Present before and after patient visits to increase engagement
-
Selected and trained to build trust with shared cultural background, common language, and health history.
-
Adept at assessing SDoH needs and offering local resources
-
Experts at navigating patients to UIH care
Create the blueprint and artifacts
With the focus on the MVP and the right partner, the rest of the work just flowed. We dove deeper with Care Coordination and co-created the service blueprint. Because service blueprint is new to the organization, we built in an orientation device to help audiences navigate different sections of the large visual. We raised the priority of the patient stories in the visual hierarchy to help audiences focus on the bigger picture from the patient's lens. Besides the poster-sized deliverable, we also created a Google slides version for presentation and collaboration as a living document.
Redesign the brochure
We didn't forget our initial charge to improve the design of the patient education brochure. We of course needed to ensure that the contents are medically accurate. Perhaps more importantly, we have to advocate for patients and make it easy to understand. As an example, we used 'high blood pressure' instead of hypertension wherever we can. We called systolic pressure 'the top number' on the blood pressure monitor. Because the brochure's role is to facilitate a face-to-face interaction, not meant to be a piece of stand-alone reading material, we kept the texts at a minimum, and used visuals when it made sense. We of course had the brochure in both English and Spanish.
What's our impact?
Introducing the hypertension action planning session
In parallel with the work above, we were running a pilot program to assess the effectiveness of the intervention. We proved that the intervention effectively lowered blood pressure. The participants became more knowledgeable about high blood pressure, and implemented more lifestyle changes to manage their blood pressure. The good results of the pilot and the research, strategy and design work done to this point secured us more funding to experiment with more iterations of the service in the following year. But more amazingly, we secured the confidence of our sponsor to roll out the MVP to multiple locations of UI Health. The concept we nurtured became the standard of care for real life patients.
What's more, we got sponsors excited about further exploring other service ideas. We came upon the ideas of community cooking class, and peer support group while talking to patients and constituents. These complementary services will serve as an extension of the action planning session to help with behavior change.
Now three years into the program, besides sustaining the program at implementation sites, we continue to work on expanding the program. Cooking class has been a great success attracting attention from insurance companies for further expansion.